Network change for some APWUHP members
Starting Jan. 1, 2024, some of your patients who are American Postal Workers Union Health Plan (APWUHP) High Option members will use the UnitedHealthcare network.*
These members will have new ID cards with the UnitedHealthcare logo on the front of the card. Please be sure to ask for the member’s ID card when they visit your office.
Sample member ID card
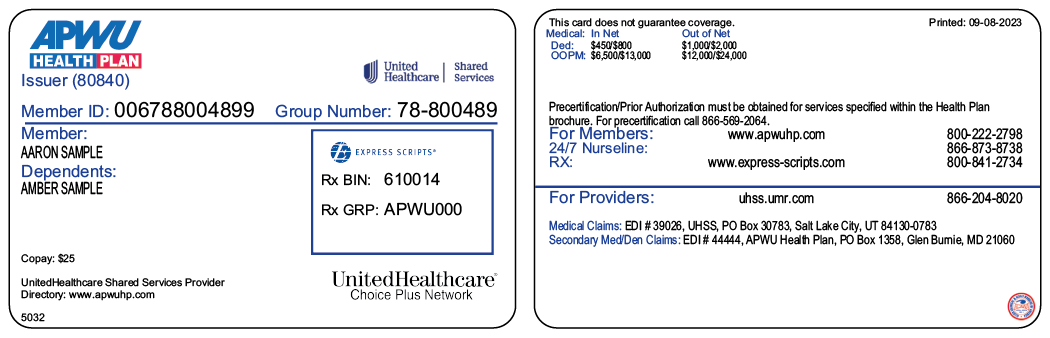
Sample member ID cards for illustration only; actual information varies depending on payer, plan and other requirements.
Member eligibility and referrals
On or after Jan. 1, 2024, you can verify eligibility at UHSS.umr.com or by calling Provider Services at 866-204-8020.
Specialists can see members without referrals, and nurse and care managers can help coordinate care for qualified members.
Submitting claims
You can submit claims in 2 ways:
- Electronic claims:
- Submit claims at UHSS.umr.com
- Medical claims: Use Payer ID 39026
- Secondary medical/dental claims: Use Payer ID 44444
- Paper claims:
- Medical claims: P.O. Box 30783, Salt Lake City, UT 84130-0783
- Secondary medical/dental claims: APWU Health Plan, P.O. Box 1358, Glen Burnie, MD 21060
Visit apwuhp.com for more information about upcoming changes to plan benefits. If you will no longer treat members transitioning to this network, please advise the member(s) to call APWUHP Member Services at 800-222-2798 for assistance with locating an in-network health care professional.
We’re here to help
If you have questions, call Provider Services at 866-204-8020, 7 a.m.–6 p.m. CT, Monday–Friday, or visit UHSS.umr.com.
*Provider network may change depending on the member’s location.
PCA-1-23-02333-UHN-NN_10162023
